Introduction to Female Sexual Dysfunction
Female sexual health is a dynamic and multifaceted phenomenon that is closely linked to a woman's overall quality of life. Sexual dysfunctions can interfere with intimacy, affect a martial relationship, and ultimately erode well-being and overall health. Determining the etiology of sexual complaints in women is often a complex process; the healthcare provider must be a cautious detective, exploring both the medical and psychological issues that can influence the sexual response cycle. An analysis of data on more than 1700 women aged 18-49 from the National Health and Social Life Survey suggested that the incidence of sexual complaints in women was approximately 43%, with diminished desire being the most frequent disorder cited.[1]
The physiology of the female sexual response involves more than the genital pelvic organs (vulva, clitoris, labia majora and minora) and the internal pelvic structures (vagina, uterus, ovaries, and fallopian tubes). The spinal and central nervous system are also major contributors as are a number of areas of the brain, including the hippocampus, hypothalamus, limbic system, and medial preoptic area. Also implicated in the response cycle are neuropeptides like serotonin, dopamine, norepinephrine, epinephrine, opioids, nitric oxide, acetylcholine, and vasoactive intestinal peptide. Sex steroids, estradiol and testosterone, are essential in the female genital response and normative functioning of the response cycle.
Etiology
There are many causes, both direct and indirect, of female sexual dysfunction. Acute or chronic bodily illness, psychological problems, and interpersonal conflicts can all have an impact on a woman's sexual response or motivation.
Biological Factors
Chronic illnesses that have been implicated in sexual dysfunction include:
- Cardiovascular diseases;
- Diabetes;
- Autoimmune syndromes; and
- Neurologic impairment.
Sexual anatomy, physiology, and normative response may also be affected by malignancy, urologic or gynecologic problems, and endocrinopathies. Estrogen depletion from natural, surgical, or chemically induced menopause, as well as premature ovarian failure,[2] may cause vaginal dryness and menopausal syndrome which can lead to sexual complaints. Young women who have either anorexia- or exercise-induced amenorrhea, bulimia, or who have had chemotherapy or radiation may also experience vaginal atrophy and sexual dysfunction.[2] Lactation-induced amenorrhea is common in women who are breastfeeding; postpartum women may also suffer from hypoestrogenemia, vaginal dryness, and atrophic complaints.
Psychological Factors
Interpersonal conflicts such as marital infidelity, as well as psychiatric illnesses such as depression, anxiety, or substance abuse, can also have an adverse effect on sexual function, as can past history of sexual abuse or physical violence. Additional factors that can contribute to sexual problems include:
- Marital discord;
- Poor partner health;
- Cultural conflicting mores;
- Lack of privacy;
- Poor relationship trust and quality;
- Poor technical skills in the partner; and
- Sexual naiveté about anatomy and orgasmic response.
Medications
In addition to acute or chronic health conditions, many medications have been implicated in detrimental sexual response. The common culprits include:
- Psychotropic medications, including antipsychotics, mood stabilizers, and
serotonin reuptake inhibitors;
- Many cardiovascular agents;
- Histamine receptor blockers; and
- Oral contraceptives.
AFUD Classification
According to the revised definitions of the American Foundation of Urological Diseases (AFUD), there are 5 categories of female sexual complaints:
- Hypoactive sexual desire disorder -- persistent or recurring
deficiency or absence of sexual fantasies, thoughts, or receptivity to sexual
activity that causes personal distress.
- Sexual aversion disorder -- persistent or recurring phobic aversion
and avoidance of sexual contact that causes personal distress and can be a
result of physical or sexual abuse or trauma.
- Sexual arousal disorder -- has many subtypes, including subjective
arousal disorder, genital arousal disorder, and combined arousal disorder.
Arousal disorders are the persistent or recurring inability to attain or
maintain sufficient sexual excitement, causing personal distress.
- Orgasmic disorder -- persistent or recurrent difficulty in delay in
or absence of attaining orgasm after sufficient sexual stimulation and arousal,
causing personal distress.
- Sexual pain syndromes -- include dyspareunia, vaginismus, and other pain disorders
| ||||||||||
Treatment: Multidisciplinary ApproachThe management of female sexual dysfunction is a complex process that requires addressing underlying medical issues coupled with treatment of psychological or psychosexual barriers. Often, several healthcare providers are involved in the dynamic treatment process for a given individual; the primary provider should have access to many specialists within his or her community. See Figure 2. 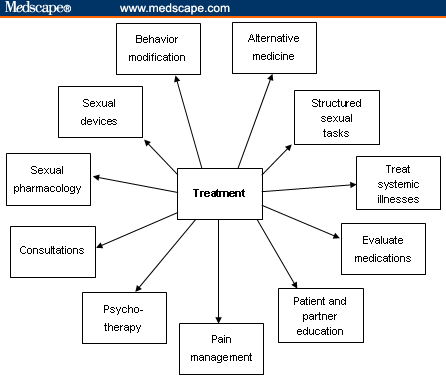 Figure 2. Treatment algorithm. Internal Medicine and PharmacologyChronic systemic illnesses, such as hypertension, hypercholesterolemia, and/or an underlying thyroid dysfunction, can be contributing factors in sexual dysfunction. Treatment of these conditions accordingly can alleviate sexual problems. Consultation with the patient's primary care provider can be very helpful. As described in the history section, careful identification of medications is also essential; antidepressants and antihypertensive medications can have effects on sexual desire, arousal, and orgasm. Occasionally, medication regimens can be modified by altering dosing and/or time intervals or specific drug classes to decrease sexual side effects. The referral to a psychopharmacologist may be necessary. Behavioral and Lifestyle ModificationsBehavioral and lifestyle modifications can improve overall quality of life and sexual function. A well-balanced diet, active exercise regime, discontinuation of tobacco use, and minimizing alcohol consumption should all be encouraged. Structured sexual tasks, such as the following, should also be encouraged:
Fatigue and poor sleep patterns may hinder sexual connectedness. The prescription should be for frequent naps or rest and instruction to plan sexual intimacy when well rested and fatigue is at a minimum. Education concerning alternate forms of sexual expression, such as mutual massage; intimate fondling and caressing; or manual, digital, or oral stimulation should also be introduced to the couple to allow for sexual exploration and enhanced sexual communication. Innovative sexual techniques or positions may help the couple reduce sexual boredom as well. Patients and their partners should be encouraged to experiment as they are comfortable with alternative sexual positions. Side-to-side or female superior position may help limit deep pelvic thrusting, which can minimize vaginal discomfort for atrophic women. It also allows for direct clitoral stimulation, which many women find pleasurable. A comprehensive sexual health program should also encourage techniques such as warm soaks to help decrease muscle tension and extensive physical therapy to help relax tense muscles. Guided imagery, quiet meditation, deep-muscle relaxation, and avoidance of lethargy are options that can be explored as well. Pain ManagementIn patients for whom pain is an element of sexual dysfunction, consultation with pain management specialists is essential. These specialists can help in adjusting opioid regimens, adding adjunctive analgesics, and modifying dosing schedules to decrease fatigue and lethargy while maintaining adequate pain relief. Patient EducationThe education of patients concerning normal genital anatomy and how the disease or therapeutic procedures have affected sexual anatomical functioning is important. The use of a handheld mirror during the pelvic examination can help the patient identify her own anatomical structures. Discussion concerning the Gräfenberg spot (G spot); clitoral, vaginal, and uterine orgasms; and dispelling some long-held sexual myths is also important. Take-home items such as pamphlets, books, videos, DVDs, and other visual aids can provide reinforcement and future reference for the patient and her partner. There are many important books on sexual exploration, and a comprehensive list of books both for erotic reading and self-education can be helpful. The American Cancer Society's booklet entitled Sexuality for Women and Their Partners[7] is an excellent patient reference guide for the patient who has sexual complaints as a result of her cancer diagnosis or treatment. Information concerning sexual devices and accessories can also be given to the patient. Sexual accessories such as self-stimulators can be encouraged as part of the sexual health treatment plan. Legitimate Web sites and Internet links should also be recommended to the patient as part of her comprehensive sexual education program. Sexual health organizations such as the International Society for the Study of Women's Sexual Health, the Women's Sexual Health Foundation, and the Alexander Foundation for Women's Health are only a few of many excellent resources. (See "Resources" at the end of this article.) Sexual TherapyCertified sexual therapists are trained to deal with patients who have:
Patients should be offered cognitive-behavioral therapy; brief intervention therapy; or marital, individual, couples, or group therapy by a trained therapist who deals with sexual issues. MenopauseThe following lifestyle changes can help manage troublesome hot flashes for menopausal women[8]:
Some nonestrogen medications (serotonin reuptake inhibitors, clonidine patch, megestrol acetate) can be used to help reduce hot flashes when systemic estrogen is contraindicated or declined by patients. LubricationNonmedicated, nonhormonal vaginal moisturizers and lubricants may be useful for women who experience vaginal dryness and painful intercourse, especially women who decline or are not candidates for minimally absorbed local vaginal hormones. Vitamin E gel capsules can be punctured with a pin and then inserted into the vagina.[9] Another method is to instruct the patient to empty the capsule's contents onto her finger and gently insert it circumferentially within the vagina. An over-the-counter polycarbophil-based vaginal moisturizing gel (Replens; Lil' Drug Store Products; Cedar Rapids, Iowa) can be used for the treatment of vaginal atrophy. When applied to the vaginal epithelium, it produces a moist film over the vaginal tissue which remains attached to the epithelial surface, providing lubrication. Replens has also been shown to restore vaginal pH measurements to premenopausal values.[10] The healthcare provider should also caution patients to read the labeled ingredients of the moisturizers. Women with severe vaginal atrophy should avoid additives in lubricants such as colors, flavors, spermicidal agents, bactericides, or warming ingredients, as these may irritate the vaginal lining.[11] Vaginal lubricants are typically used during sexual intercourse, and many people who use them find that they enhance sexual intimacy. A good lubricant should be water-based and compatible with rubber products like diaphragms or condoms. Lubricants should be easy to apply within the vagina. They can typically be purchased in the pharmacy, grocery store, or online. When using lubricants, it is suggested to have a small hand towel close by for easy clean-up. Many lubricants require reapplication during intercourse, so patients should be advised to keep the bottle handy for reapplication. Petroleum-based products such as mineral oil, petroleum jelly, and edible oils should be avoided within the vaginal vault; they can interfere with helpful vaginal bacteria, can disrupt the bacterial balance, and have also been known to weaken condoms. Sexual DevicesSexual devices such as vaginal dilators or self-stimulators are helpful when vaginal shortening or narrowing has occurred. Scar tissue can impede penetration, causing dyspareunia. Vaginal dilators with lubricants can help lengthen and widen the vagina and loosen the scar tissue that may contribute to tenderness and distress associated with vaginal intercourse. Ongoing supportive physical therapy is essential, and often behavioral therapy can be influential for continued compliance. The Eros (UroMetrics; St. Paul, Minnesota) clitoral stimulator has been prescribed for patients who have had cervical cancer and for some with intravaginal radiation. Others who have used the device with success include those with other pelvic cancers, such as rectal and vaginal cancers. The Eros stimulator is the only device currently approved by US Food and Drug Administration (FDA) for the treatment of female sexual complaints. It is a battery-operated device with a suction cup that fits around the clitoris and facilitates engorgement. The device is expensive, but if the diagnosis is clearly documented in the patient's chart, insurance will often cover the cost. Pharmacotherapy: EstrogenSexual pharmacology remains the mainstay of treatment for many female sexual complaints. A number of healthcare providers advocate systemic hormonal therapy with estrogen, progesterone (if the woman has a uterus to prevent endometrial hyperplasia), and varying degrees of supplemental testosterone. The discussion of hormonal therapy is beyond the scope of this article and the reader is referred to the North American Menopause Society or the American College of Obstetricians and Gynecologists for further product selection and specific choice details. The Women's Health Initiative (WHI) results sparked much controversy and have had an impact on patient perception of hormonal therapy and physician prescribing patterns.[12,13] Many women are fearful of systemic estrogen therapy because of the increased risk for breast cancer and cardiovascular effects; many are opting for minimally absorbed local estrogenic therapies that can effectively treat vaginal complaints. In 2003, the FDA stated that local estrogen therapy should be used for the treatment of moderate-to-severe symptoms of vulvar and vaginal atrophy.[14] There have been some concerns over long-term safety with hormonal therapy in light of the WHI studies, and many patients and healthcare providers are now exercising caution before prescribing hormones. A risk-benefit analysis is often undertaken with the participation of the patient and is documented in the patient chart. Each patient must assess the personal risk of hormones vs the benefits. Local vaginal hormones come in a variety of different application methods. Creams, rings, and tablets are the most common types of minimally absorbed vaginal estrogen products that are presently available.[15] See the Table for their dosing schedules. Table. Vaginal Estrogen Therapy
Adapted from: Pinkerton J. Vaginal estrogen therapy: The question of systemic absorption. Female Patient. 2006;31:24-26. Vaginal creams. Vaginal creams contain either conjugated estrogens or estradiol and are typically applied to both the interior of the vagina and exterior of the vulvar vault with an applicator that can be refilled and reused. Patients self-administer the quantity, and some women find creams especially soothing to the pelvic region. Others may find them messy because the cream may leak and drip. Vaginal ring. The 17 beta-estradiol-releasing vaginal silicone-plastic ring is a minimally absorbed vaginal ring that is placed within the vault every 3 months. The vaginal ring is typically inserted by the healthcare professional in an office setting to ensure that the ring is placed in the upper third of the vaginal vault. The patient can reinsert the ring on a 3-month basis or if it is expelled for any reason. The 2.0-mg dose of estradiol is released over a 3-month period. Some women find this product extremely helpful because they do not have to remember to use it on a daily basis. Others, however, find it uncomfortable, and some partners have even complained of feeling the ring during sexual intercourse. Vaginal erosions or abrasions have been associated with the vaginal ring which may also be expelled during urination, defecation, or intercourse. Some women report an increase in vaginal discharge while using the ring. Vaginal tablets. Minimally absorbed vaginal tablets (17 beta-estradiol) are another option for local vaginal estrogen therapy. The tablets are contained in a prefilled plastic applicator which is disposable and biodegradable. These tablets, which patients self-administer twice a week, are well tolerated and not associated with increased incidence of endometrial hyperplasia.[16] Advantages of this system are that it is inconspicuous, convenient to use, and does not cause a mess. A study of this system by Suckling and coworkers[17] demonstrated success rates in excess of 85% of women treated. Pharmacotherapy: AndrogensOne common but still controversial treatment for female sexual dysfunction is androgen therapy. Oral esterified estrogen with methyl-testosterone has been used in the field of sexual medicine extensively since the 1970s but it has yet to win FDA approval for the treatment of desire issues.[18] The testosterone transdermal patch was recently approved for hypoactive sexual desire disorder (HSDD) in Europe, but there is no approved medication in the United States. The long-term safety and efficacy of androgen therapy has not yet been established, but there is increasing evidence that testosterone therapy has beneficial effects on libido, mood, and bone mineral density.[19-21] One long-term safety issue is a concern that the testosterone can be aromatized to estrogen, which may reactivate or promote breast cancer cell tumor growth. Alexander and colleagues[22] published an excellent review of the available medical data of testosterone and libido in surgically and naturally menopausal women. The review systematically examined evidence from randomized controlled trials (RCTs) and reported that there seems to be value in giving testosterone to estrogen-replete menopausal women with desire concerns. Kinsberg[23] discussed the INTIMATE (Investigation of Natural Testosterone in Menopausal women Also Taking Estrogen) studies, which demonstrated that transdermal testosterone is a safe and effective treatment with minimal side effects for HSDD. The new testosterone transdermal matrix patch Intrinsa (Procter & Gamble; Cincinnati, Ohio) is a promising treatment for low libido; however, further RCTs and safety data are warranted before considering use in patients with this problem. Other agents in differing clinical stages of development include: Flibanserin. This is a 5H1-agonist/2A antagonist manufactured by Boehringer Ingelheim for the treatment of HSDD. This agent is believed to be well tolerated and is associated with minimal side effects, including nausea, dizziness, fatigue and somnolence, and increased bleeding when taken along with nonsteroidal anti-inflammatory drugs or aspirin. Phase 3 clinical trials are presently under way. Alprostadil. This is a naturally occurring potent vasodilator that has an important role in the regulation of blood flow to the female reproductive tract. Local application may increase vaginal blood flow and sensation, leading to increased sexual arousal. Several trials are under way. Alpha-melanocyte-stimulating hormone (MSH) analog: PT-141: bremelanotide. This agent is administered as an intranasal spray. It is in development for the treatment of female sexual dysfunction. Tibolone. This agent, which is currently unavailable in the United States, is thought to reduce hot flashes, increase bone mineral density, and have a positive effect on vaginal dryness. It may also improve desire but not sexual function. Studies of the impact of tibolone on lipid metabolism and hemostasis are inconclusive, and long-term effects remain unknown. Nonmedical Pharmacotherapy: Over-the-Counter SupplementsIn addition to the agents mentioned above, many nonpharmacologic therapies are being marketed directly to the consumer as sexual health enhancers. Besides having worrisome and potentially detrimental side effects, very few of these supplements have been shown in randomized trials to have any clinical effect on sexual dysfunction. Some patients may experiment with foods that are traditionally thought to enhance sexuality, such as chocolate, ginseng, oysters, and black cohosh. Although these foods are unlikely to cause adverse events, their efficacy has not been established in controlled studies. Various combination over-the-counter alternatives are also popular but have not been properly studied. DHEA. Another popular alternative substance, DHEA, has limited RCT data.[24] According to one placebo-controlled trial, raising levels of DHEA via supplementation improved frequency of sexual thoughts, sexual interest, and sexual satisfaction. DHEA has been shown to increase androgens, decrease high-density lipoprotein, and decrease sex hormone binding globulin. However, high levels of DHEA have been correlated with increased risk for cardiovascular disease in women. Consultants: Multidisciplinary ManagementConsultants are a critical element in the comprehensive multidimensional management of the female sexual health patient. Some of the many healthcare providers included in the dynamic may be:
A list of clinicians and ancillary staff who are sensitive to sexual issues should be readily available for patients who take part in sexual health programs. |
Follow-up and Maintenance
Routine follow-up of patients on local estrogen vaginal therapy and hormones is warranted to ensure efficacy and correct dosing of prescribed treatment. Ongoing evaluation and management is appropriate to assess for resolution of distressing symptoms. For those on androgen therapy, careful surveillance is advocated along with repeat bloodwork done at intervals to monitor for side effects
The diagnosis and treatment of female sexual complaints is a complex, multimodal medical psychological health concern which warrants assessment and comprehensive therapeutic modalities to achieve success and resolve complaints.
No comments:
Post a Comment